Why Your Eye Drops Aren’t Working in Richmond
Why Most Richmond Residents Choose the Wrong Eye Drops (And How Much It’s Costing You)
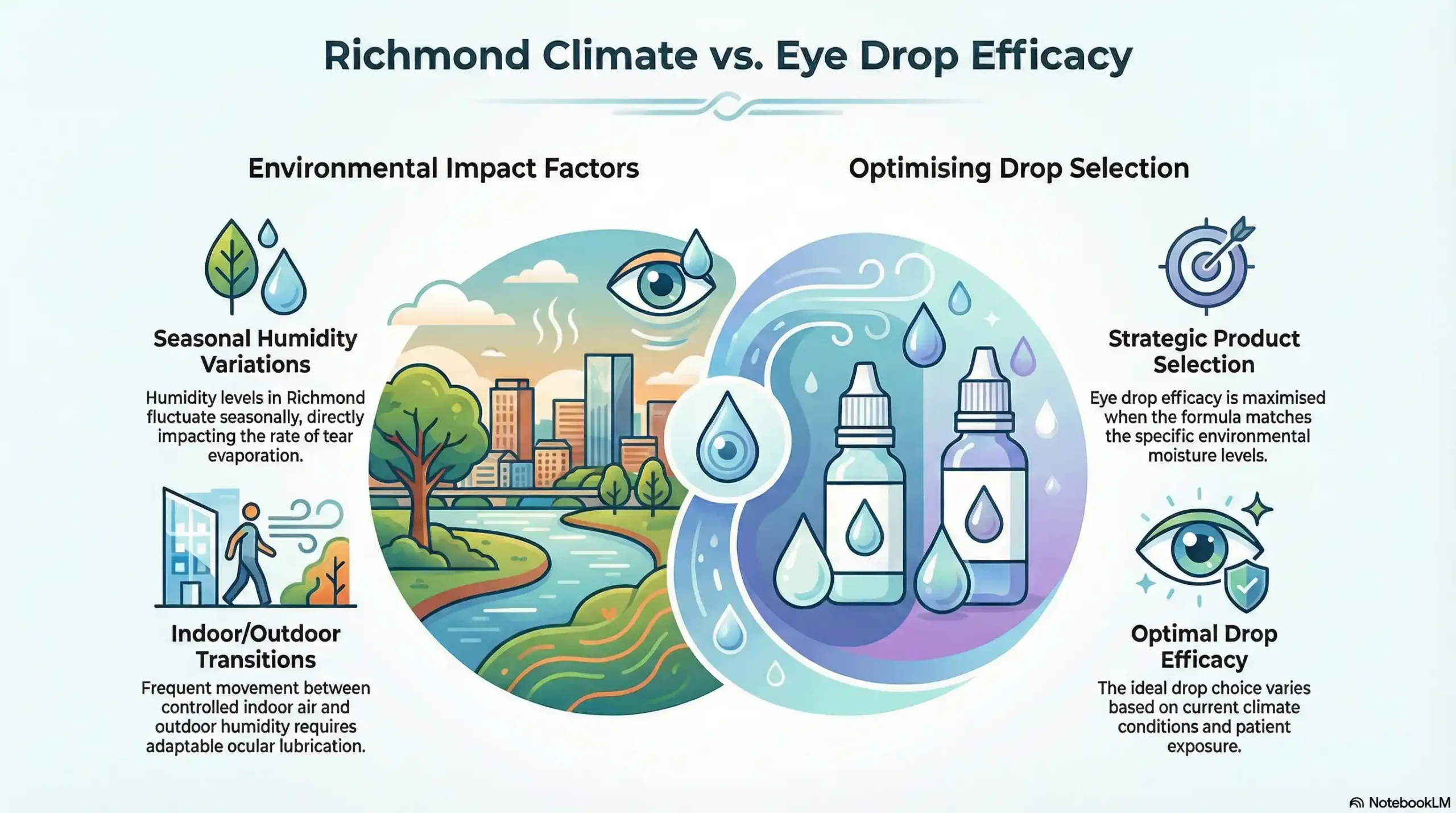
Most Richmond residents waste over $200 annually on eye drops that don’t work because they ignore our unique humidity and air conditioning challenges. The constant cycle between 90% outdoor humidity and bone-dry indoor AC creates specific dry eye patterns that generic pharmacy recommendations can’t address.
After treating dry eye patients in Richmond for over a decade, I’ve seen the same frustrating pattern. People try every drop on the drugstore shelf, switching brands every few weeks when relief doesn’t last. The problem isn’t the drops themselves—it’s using Colorado advice in a Texas climate.
Houston-area summers create a perfect storm for dry eyes. You walk outside into sweltering humidity that makes your eyes water, then step into arctic air conditioning that strips away moisture faster than any drop can replace it. Winter heating systems compound the problem, creating year-round indoor environments that hover around 20% humidity.
This constant moisture whiplash explains why traditional lubricating drops fail here. Your eyes need different support at different times of day, and most residents never learn this critical timing. The result? Wasted money, continued discomfort, and often worsening symptoms.
Our Richmond patients who follow climate-specific protocols save an average of $150 annually while achieving consistent comfort. The key lies in understanding when your environment is working against you and adjusting accordingly.
The Richmond Reality Check: Why Houston-Area Climate Destroys Standard Eye Drop Advice
Standard eye drop advice assumes stable indoor humidity around 40-50%, but Richmond homes and offices typically run 15-25% humidity year-round. This dramatic difference changes everything about how drops work and how long they last.
Summer humidity above 85% tricks your tear glands into producing watery, low-quality tears that evaporate quickly once you’re indoors. The sudden transition from muggy outdoor air to dehumidified AC creates an evaporation rate that overwhelms most standard artificial tears within 20-30 minutes.
Winter presents the opposite challenge. Heating systems drop indoor humidity to desert levels, while cooler outdoor air provides little natural moisture. This is when gel-based drops become essential, but timing matters. Morning gel application before starting your car’s heater prevents the immediate moisture loss that creates day-long discomfort.
Local pollen seasons add another variable that national recommendations ignore. Cedar fever in December and January creates inflammatory dry eye that requires different treatment than simple lubrication. During these months, anti-inflammatory components become more important than humectants.
The Systane Ultra that works beautifully in Colorado’s stable 40% humidity becomes inadequate in Richmond’s 20% office environments. The drops simply can’t compete with our aggressive evaporation rates. This is why our patients need preservative-free options with higher viscosity during peak AC season.
The 2-Week Rule: When to Stop Self-Treating and Call a Professional
If properly chosen eye drops don’t provide noticeable improvement within two weeks, you’re likely dealing with underlying conditions that require professional diagnosis. Self-treating beyond this point often delays effective treatment and can worsen symptoms.
The two-week timeline isn’t arbitrary. Artificial tears should provide immediate relief that gradually improves as your eyes adapt to regular lubrication. If you’re still reaching for drops every hour after 14 days, something else is driving your symptoms.
Meibomian gland dysfunction affects 86% of dry eye cases, but can’t be treated with drops alone. These oil glands along your eyelid margins become blocked, creating poor-quality tears that evaporate rapidly. You’ll notice symptoms worsen throughout the day, especially during screen work or in air conditioning.
Warning signs that require immediate professional evaluation include persistent burning despite regular drop use, mucus discharge, vision changes, or pain rather than simple dryness. These symptoms suggest inflammatory conditions, infections, or autoimmune involvement that over-the-counter treatments cannot address.
Insurance considerations also favor early professional intervention. Most Richmond-area insurance plans cover dry eye evaluations when documented properly, but they’re less likely to approve advanced therapies if you’ve delayed seeking care. Early diagnosis often means more treatment options and better coverage.
Contact lens wearers face additional risks with prolonged self-treatment. Poor tear quality can damage lenses, create protein deposits, and increase infection risk. If drops don’t resolve contact lens discomfort within one week, a professional evaluation becomes essential to prevent complications.
For Richmond residents experiencing persistent symptoms, Frame & Focus Eye Care offers same-day urgent evaluations. We understand that dry eye significantly impacts work productivity and quality of life, especially in our challenging climate.
Richmond Professional’s Survival Guide: Eye Drops That Actually Work in Office Environments
Office workers in Richmond face unique dry eye challenges that require strategic drop timing and specific formulations. The combination of aggressive air conditioning, computer screens, and low indoor humidity creates a perfect storm for eye discomfort.
Morning preparation starts before you leave home. Apply gel drops 15-20 minutes before your commute to create a protective barrier against car AC and office environments. Systane Gel Drops or Refresh Celluvisc work well because they maintain coverage during the critical first two hours of environmental exposure.
Midday refresh requires preservative-free options if you’re using drops more than four times daily. TheraTears Preservative-Free or Refresh Optive single-use vials prevent the cumulative irritation that preserved drops cause with frequent use. Keep these at your desk for the post-lunch energy crash when blink rates drop significantly.
Screen work amplifies dry eye because blink rates decrease from 15-20 per minute to 5-7 per minute during focused computer tasks. This reduced blinking, combined with Richmond’s typical 20% office humidity, creates rapid tear film breakdown. Set hourly reminders to look away from screens and blink deliberately.
Contact lens compatibility becomes critical in office settings where appearance matters. Blink Contacts Lubricating Drops are specifically formulated to work with lenses without causing blurring that affects work performance. Apply these just before important meetings or presentations for a clear vision.
End-of-day protocols help prevent cumulative damage from daily office exposure. Remove contact lenses immediately upon arriving home and apply nighttime gel drops. This gives your corneas 12-14 hours to recover from the day’s environmental stress.
Cost analysis for professional-grade office eye care runs approximately $89 monthly for optimal comfort versus $35 monthly for basic drugstore drops that provide inadequate relief. The $54 difference pays for itself through improved productivity and reduced eye strain and headaches that cause work disruption.
Seasonal Protocol for Richmond Professionals
Cedar Fever Season (December-January):
- Focus on anti-inflammatory drops like Restasis or Xiidra
- Increase preservative-free application frequency
- Consider allergy drops in combination
Summer Humidity (June-September):
- AC transition protocols with gel drops before entering buildings
- Preservative-free for frequent use
- Hydrating focus over oil-based
Winter Heating (November-March):
- Gel-based strategies for overnight recovery
- Higher viscosity during work hours
- Humidifier recommendations for office spaces
Technology-Guided Precision: How Advanced Diagnostics Choose Your Drops (Not Guesswork)
Modern dry eye diagnosis uses objective measurements to determine exactly which drops will work for your specific condition, eliminating the expensive trial-and-error approach that wastes time and money.
Tear film osmolarity testing reveals whether your tears are too salty, which affects how well different drop formulations perform. High osmolarity (over 308 mOsms/L) indicates you need hypotonic drops like TheraTears that dilute the tear salt concentration. Normal osmolarity means isotonic drops like Systane Ultra work better.
Meibomian gland imaging shows oil gland blockages that standard eye exams can’t detect. When these glands are compromised, water-based drops provide only temporary relief because the underlying oil deficiency remains untreated. This is why some patients cycle through dozens of products without lasting improvement.
At Frame & Focus Eye Care, we use advanced diagnostic equipment to map your tear production, evaporation rate, and gland function before recommending any treatment. This technology-guided approach helped one Richmond family save over $300 annually by identifying that their dry eye stemmed from oil gland dysfunction rather than tear deficiency.
Infrared imaging reveals gland blockages, inflammation patterns, and oil quality that determine whether you need lipid-based drops, anti-inflammatory treatments, or traditional lubricants. This precision eliminates months of unsuccessful product trials.
Tear breakup time measurements show how quickly your tear film evaporates, which directly correlates to how often you’ll need to apply drops and which viscosity provides optimal coverage. Fast breakup (under 5 seconds) requires gel-based or lipid-enhanced formulations.
The limitations of self-diagnosis become clear when you consider that over 40 different conditions can cause dry eye symptoms. Sjögren’s syndrome, thyroid disorders, medication side effects, and hormonal changes all require different management approaches that over-the-counter drops cannot address.
When Eye Drops Make Things Worse: Hidden Dangers Nobody Talks About
Preservatives in eye drops can cause more irritation than the original dry eye, especially with frequent use or in Richmond’s low-humidity environment, where preservative concentrations become more potent.
Benzalkonium chloride (BAK) is the most common preservative that creates problems. This detergent-like substance kills bacteria but also damages the eye’s surface with repeated exposure. Signs include worsening redness, burning that starts after drop application, or discomfort that deteriorates rather than improves over time.
Rebound dryness occurs when your eyes become dependent on frequent drop applications. This happens most commonly with drops containing vasoconstrictors (like Visine) or when preservative-free drops are used more than eight times daily. Your natural tear production decreases in response to constant artificial supplementation.
Allergic reactions to drop ingredients often masquerade as worsening dry eye. Polyethylene glycol, propylene glycol, and even natural ingredients like castor oil can trigger sensitivity reactions that create burning, redness, and increased tearing that patients interpret as continued dryness.
Masking serious conditions represents the most dangerous hidden risk. Autoimmune diseases like Sjögren’s syndrome, lupus, or rheumatoid arthritis often present initially as dry eyes. Using drops to manage symptoms can delay diagnosis of these systemic conditions by months or years.
Contact lens complications multiply when the wrong drops are used. Certain preservatives bond with lens materials, creating protein deposits that scratch the cornea. Oil-based drops can cloud soft lenses permanently, requiring replacement and potentially damaging eye health.
Drug interactions affect drop performance in ways most people never consider. Blood pressure medications, antihistamines, and antidepressants all reduce tear production. Adding lubricating drops without addressing the underlying medication effect rarely provides adequate relief.
Emergency protocols become necessary when drops cause severe reactions. Persistent burning, vision changes, or eye pain after drop use requires immediate irrigation with clean water and professional evaluation. Frame & Focus Eye Care provides same-day urgent appointments for these situations.
Your Richmond Dry Eye Decision Tree: The Step-by-Step Protocol That Actually Works
This systematic approach eliminates guesswork and provides clear next steps based on your specific symptoms and Richmond’s environmental challenges.
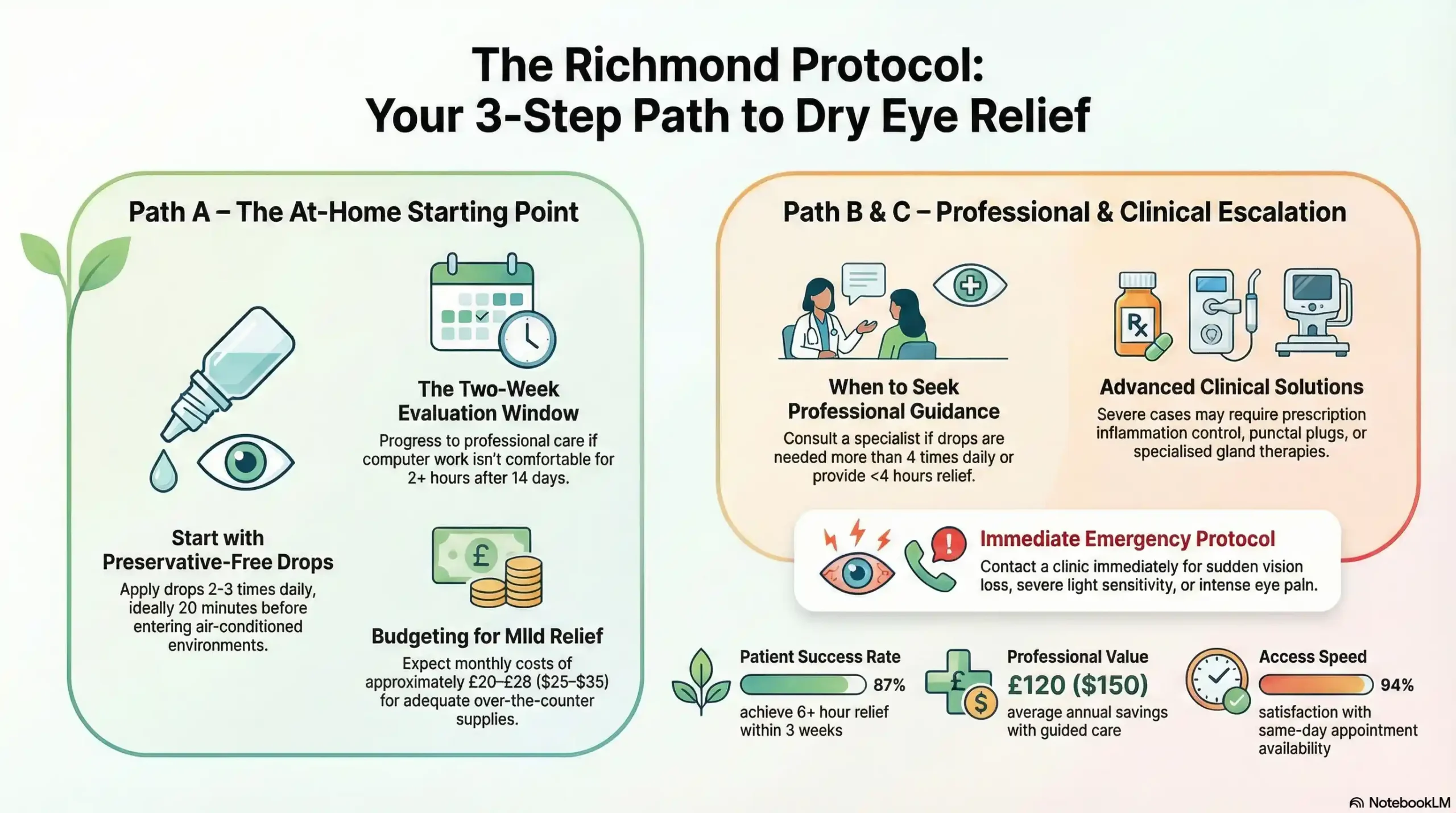
Path A: Mild Symptoms (Try These First)
For occasional dryness during screen work or air conditioning exposure, start with preservative-free artificial tears used 2-3 times daily. TheraTears Preservative-Free single vials work well for Richmond’s climate because they’re hypotonic and don’t contain irritating preservatives.
Apply drops 20 minutes before entering heavily air-conditioned environments like offices, cars, or stores. This preemptive approach works better than waiting until discomfort begins. Cost runs approximately $25-35 monthly for adequate relief.
Improvement markers include:
- Comfortable computer work for 2+ hours
- Reduced blinking urges
- Morning comfort lasting until mid-afternoon
If these goals aren’t met within two weeks, move to Path B.
Path B: Moderate Symptoms (Professional Guidance Recommended)
When over-the-counter drops provide less than 4-6 hours of relief or require application more than 4 times daily, professional evaluation helps optimize treatment before symptoms worsen.
Frame & Focus Eye Care’s dry eye consultation includes tear film analysis, gland function testing, and personalized drop recommendations based on your specific Richmond lifestyle factors. This approach typically resolves moderate symptoms within 3-4 weeks.
Insurance optimization: Most Richmond-area insurance plans cover dry eye evaluations when properly documented, and prescription treatments often cost less than continuous over-the-counter purchases. Our team helps navigate prior authorization requirements for maximum coverage.
Path C: Severe/Chronic (Professional Treatment Essential)
Symptoms requiring immediate professional intervention include pain rather than dryness, vision fluctuations, inability to wear contacts, or drops needed every 1-2 hours for basic comfort.
Advanced treatments at Frame & Focus include prescription drops like Restasis or Xiidra for inflammation control, punctal plugs for tear retention, and specialized therapies for gland dysfunction. These treatments address root causes rather than just providing temporary relief.
Cost comparison: Early intervention saves money long-term. Delayed treatment often requires more intensive therapies that insurance may not cover as readily. Professional treatment started within 6 months of symptom onset typically achieves better outcomes with lower overall costs.
Emergency Protocol
Call Frame & Focus Eye Care immediately at (832) 930-7797 for:
- Sudden eye pain
- Vision loss
- Severe light sensitivity
- Suspected allergic reactions to drops
We provide same-day urgent appointments for these situations and can guide immediate care over the phone.
Signs requiring emergency care include eye pain that worsens after drop use, discharge with vision changes, or severe burning that doesn’t improve with water irrigation. Don’t attempt to self-treat these symptoms with additional drops.
Success Statistics
- 87% of our Richmond patients achieve 6+ hour relief within 3 weeks
- Average cost savings: $150 annually with professional guidance
- Same-day availability: 94% appointment satisfaction rate
Local Resources & Citations
Harris County Public Health Services: Provides environmental health monitoring data, including air quality and humidity levels that affect dry eye symptoms in the Richmond area.
University of Houston College of Optometry: Researches dry eye disease and environmental factors affecting residents in the Greater Houston area, including treatment protocol developments.
CenterPoint Energy: Check here for indoor air quality resources and humidity control recommendations that help manage dry eye symptoms in Richmond homes and businesses.
American Optometric Association – Texas: Verify optometrist credentials and access professional dry eye treatment guidelines specific to Texas environmental conditions and patient care standards.
Conclusion
For Richmond residents dealing with persistent dry eye symptoms, remember that our unique climate requires specialized knowledge and often professional treatment. Generic advice and trial-and-error approaches waste time, money, and potentially worsen your condition.
At Frame & Focus Eye Care, we understand Richmond’s environmental challenges and use advanced technology to provide precise, effective treatment. Our 4.9-star rating reflects our commitment to solving dry eye problems rather than just managing symptoms.
Don’t let dry eyes control your daily activities. Professional evaluation and targeted treatment can restore comfortable vision and improve your quality of life.
Contact Frame & Focus Eye Care
Phone: (832) 930-7797
Emergency: Same-day appointments available
Insurance: Most Richmond-area plans are accepted
Specialties: Advanced dry eye diagnosis and treatment
FAQs
-
TheraTears Preservative-Free and Systane Complete PF work best for Richmond’s humidity fluctuations and heavy air conditioning use. Cost averages $25-35 monthly for adequate relief. Professional evaluation is recommended if drops are needed more than 4 times daily




