Everything You Need to Know About Demodex Mites
Do you suffer from persistent eyelid itching or chronic dry eyes? The hidden cause could be the Demodex mite. Learn the surprising symptoms and specialized treatments that restore comfort and eye health.
Key Takeaways for Your Eye Health
-
Look Beyond Dry Eye: Persistent itching, burning, and the feeling of a foreign body in the eye may be caused by Demodex mites, not just typical dry eye.
-
A Cylindrical Clue: The most visible early sign of infestation is cylindrical dandruff (CD)—waxy debris at the base of the lashes.
-
Age and Immunity are Factors: Demodex prevalence increases with age and is a higher risk for individuals with compromised immune systems (e.g., diabetics, long-term steroid users).
-
Diagnosis requires a Doctor: Mites are microscopic. Accurate diagnosis requires professional evaluation, typically through a slit-lamp exam or microscopic viewing of an epilated eyelash.
-
Treatment is a Process: Effective treatment involves specialized in-office débridement and a mandatory 2-week follow-up for repeat treatment, not just over-the-counter remedies.
-
Home Hygiene is Critical: Successfully eliminating mites requires immediate and weekly washing of bedding in hot water and daily use of non-soap cleansers on the face and eyelids.
-
Ditch the Grease: Avoid oil-based cleansers, greasy makeup, and lotions, as these provide “food” for the mites and can encourage their population growth.
What Is Demodex?
The Demodex mite is a type of parasite that lives on humans and can reside in hair follicles and sebaceous glands. These mites are arachnid (eight-legged) and invisible to the naked eye, varying in size from 0.1mm to 0.4 mm long. They typically live on the face and in the hair follicles of the eyebrows, eyelids, roots of the eyelashes, facial hair, and around the ears and are associated with various skin problems of the eyes and face, such as blepharitis and acne rosacea.
Demodex can affect humans at any age, but its prevalence increases in prevalence with increasing age. Immunity-compromised patients, such as diabetics, patients on long-term corticosteroids or chemotherapy, or patients who have HIV/AIDS, also have increased risk and prevalence of Demodex infection. Usually, when the immune system is weakened and the parasitic population has colonized, this disease can badly damage the skin.
How Can Demodex be Transmitted?
For transmission of mites from one person to another, direct contact of hair and sebaceous glands on the nose, or dust containing eggs is required. Since the disease processes begin when there is an overpopulation of Demodex, the vast majority of cases of mites go unobserved and don’t show any adverse symptoms. However, in certain cases, the mite populations migrate and multiply in the eyelashes.
What Are The Types of Demodex?
There are two existing types of Demodex mites: the longer kind, Demodex folliculorum, which live in the hair follicles, and the shorter ones, Demodex brevis, which live in the sebaceous (oil) glands in the skin.
What Are The Symptoms of Demodex?
In the early stages, there are often no noticeable symptoms, but if left untreated, Demodex can progress. Symptoms vary among patients and may include dry eye, red eyes, severe itching along the eyelid margin and eyebrow, especially in the morning, eyelid irritation, burning sensation, foreign body sensation that seems to originate beneath the eyelids, heavy lid, and blurry vision. One of the earliest signs of mite infestation is cylindrical dandruff (CD), which is the accumulation of fine, waxy, dry debris that collects at the base of the lash and extends up to 2 mm along the length of the lashes and is most noticeable on the upper lashes.
How Is Demodex Diagnosed?
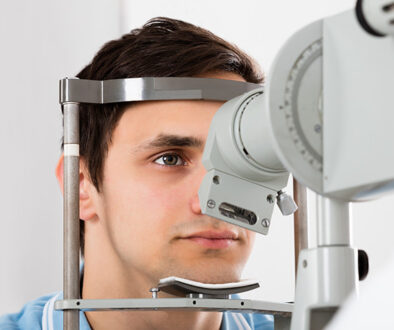
Demodex mites can be diagnosed by a slit-lamp evaluation or by carefully removing and viewing an epilated eyelash under the microscope.
How Is Demodex Treated?
Initial treatment involves an in-office lid scrub/débridement, which starts with a drop or two of long-lasting anesthetic being instilled. The lashes and eyebrows are then thoroughly débrided. Next, an antibiotic/steroid ointment is applied to help keep the mites from moving and also possibly suffocate them. The steroid also helps in calming down the inflammation secondary to the chemical and mechanical irritation of the in-office treatment, in addition to suppressing any possible inflammatory cascade associated with the decaying mites. The patient should return in 2 weeks and repeat the in-office treatment.
What Are The Instructions for Patients with Demodex?
The patients diagnosed with Demodex need to know a few simple instructions:
- Immediately wash bedding and pillowcases in hot water and dry in a heated dryer before beginning treatment, and once a week thereafter.
- Wash face, nostrils, hair, external ear, and neck with a non-soap cleanser twice daily.
- Scrub the eyelids with a mild (baby) shampoo.
- Avoid using makeup for at least 1 week and discard all old makeup.
- Avoid oil-based cleansers, greasy makeup, lotions, and sunscreens, which can provide further “food” for the mites.
- Exfoliate your face once or twice a week to remove dead skin cells and trapped sebum. Keep pets away from sleeping surfaces.
The Nocturnal Life of Demodex: Why Your Symptoms Peak at Night
While you sleep, the microscopic world on your eyelids is at its most active. Demodex mites are photophobic, meaning they are highly sensitive to light. During the day, they remain buried deep within your hair follicles or oil glands to avoid UV rays.
However, as soon as the lights go out, these mites emerge to the skin’s surface to mate and migrate. This “night shift” is the primary reason why many of our Richmond patients wake up with:
-
Intense morning itching along the lash line.
-
“Crusty” eyes or waxy debris (cylindrical dandruff) that appears overnight.
-
Red, swollen lids caused by the inflammation triggered by their nighttime movement.
Dr. Zaver’s Insight: Because of this 14-to-18-day reproductive cycle, we don’t just treat you once. We schedule follow-ups to catch the next generation of mites before they can restart the cycle. If you are experiencing these “frightening” morning symptoms, our emergency eye care team is available for same-day evaluations.
The Demodex-Rosacea Connection: When “Friendly” Mites Become Pathogens
Almost everyone has a small population of Demodex mites—they are technically a natural part of our skin’s microbiome. However, for those suffering from ocular rosacea, the relationship turns toxic.
Recent clinical reviews highlight a “vicious cycle” where rosacea-prone skin provides the perfect oily environment for mites to overpopulate. Once the population hits a tipping point, they stop being harmless and start acting as vectors for bacteria like Bacillus oleronius. When these mites die, they release bacteria that trigger a massive inflammatory response, leading to the “gritty” feeling often mistaken for standard dry eye.
Better Vision Tip: If your eyes feel like “sandpaper,” you may need more than just artificial tears. Explore our specialized dry eye treatments to address the root inflammatory cause.
Modern Medical Breakthroughs: The New Gold Standard for Relief
For years, the only real home remedy was tea tree oil, which can be harsh and irritating to the eyes. In 2025, we will have moved toward targeted, FDA-approved clinical solutions that work faster and more comfortably.
-
Xdemvy (Lotilaner): This is the first and only prescription drop designed to paralyze and eliminate Demodex mites directly.
-
IPL (Intense Pulsed Light): We use light energy to eliminate mites and clear out the oil glands. This is a game-changer for patients who want to move beyond daily lid scrubs.
-
Lid Debridement: In our office, we use professional tools to manually clear away the “collarettes” or dandruff that mites leave behind, giving your eyelids a fresh start.
Expert Note: These advanced treatments are part of our commitment to using state-of-the-art technology to protect your vision.
Your “Mite-Proof” Long-Term Maintenance Plan
Success isn’t just about killing the current population; it’s about making your eyelids an “unfriendly” environment for future mites. Here is your 2025 maintenance checklist to prevent a relapse:
-
The Hypochlorous Acid Rule: Use a medical-grade cleansing spray daily to keep bacteria levels low.
-
Makeup Hygiene: If you’ve had an infestation, discard your old mascara and eyeliner immediately. Mites can hitch a ride on beauty tools! Check out our guide on choosing the right frames and eye-safe products for more tips.
-
Contact Lens Care: If you wear contact lenses, ensure you are following a strict disinfection protocol, as mites can thrive around poorly cleaned lens cases.
-
Heat & Hygiene: Wash your pillowcases in hot water (140°F) at least once a week to kill any stray eggs or mites.
Sources & Further Reading
For a deeper understanding of Demodex mites and ocular surface disease, you can refer to the following clinical and educational resources:
-
[Source 1: General Ocular Demodex Information]
American Academy of Ophthalmology: Blepharitis and Mite Infestation - [Source 2: Clinical Treatment Protocols]
National Library of Medicine (NIH): Management of Ocular Demodicosis
With the proper medical care, treatment, and hygiene, the Demodex count usually drops to zero in 4-6 weeks without recurrence in the majority of cases. Patients receiving therapy show dramatic improvements in symptoms, eye inflammation, tear film stability, and vision.
Ready to see clearly again? Don’t let itchy eyes ruin your day. Whether you’re in Richmond, Sugar Land, or Pecan Grove, Dr. Zaver and the team at Frame & Focus Eye Care are here to help you feel like family while receiving world-class care.
FAQs
-
Demodex is a microscopic eight-legged parasite (0.1–0.4mm). It lives primarily in the hair follicles and sebaceous glands of your eyelids, eyelashes, and face.